2013: Scientific Workshop Summary
October 4 – 5, 2013
(ILC/DDD-EDS-CANADA)
 Influencing change through experience:
Influencing change through experience:
- Canada’s first Ambassador of Hope for Ehlers-Danlos Syndrome – Brooklyn Mills
- National awareness through communications with ILC’s medical advisors who comprise Canada’s leading pain experts who remarked at December 2012 Medical Advisory Board Meeting that they owe ILC and EDS a debt of gratitude in helping them to recognize the need to take a broad view of connective tissue disorders to understand the complexities of chronic pain illness.
- We learned that medical best practices do not exist for the diagnosis, treatment and care of a broad group of complex chronic pain diseases including, Ehlers-Danlos Syndrome; and therefore wrote the Difficult to Diagnose Disease Program modeled after the Undiagnosed Disease Program through the National Institute of Health Research which has been accepted as important and template-able to many needs.
- In January 2013 ILC was invited to attend a meeting with Ministry of Health (MOH) representatives Pauline Ryan, Dr. Gary Salisbury and Julie Ingo where we were told that there is work being done as a strategy for chronic pain in adults but they did not have chronic pain in children on their radar. We reported on the ILC’s overall vision and mission including the Difficult to Diagnose Disease Program. Following this meeting a large round table meeting took place with Ontario Children’s hospital representatives with sub-committees created with invitation to report on needs with follow up meeting that took place during the month of May.
- To date, through peer support the ILC have connected with over 150 individuals that live with EDS that continuously fall between the cracks of care.
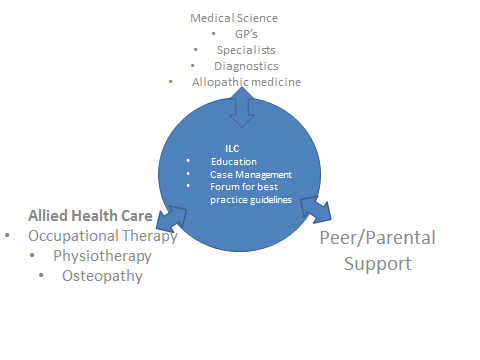
- Oakville, Ontario – October 4th and 5th, 2013, the ILC hosted a Scientific Workshop for thought leaders to begin the process of bridging gaps in best practices, attended by twenty-six medical and allied health professionals from Halton, Hamilton, London, the GTA, Quebec and the United States. The outcomes of this cohesive collaboration will, in the fullness of time, bridge these gaps and bring better care to those that suffer tremendously.
Scientific Workshop Outcomes
The ILC Difficult to Diagnose Disease Program (“DDD Program”) *TM pending
Developing Best Care Practices for Complex Chronic Pain Diseases
![]()
![]()
![]()
Bridging Scientific Gaps: Expert Leadership and Vision
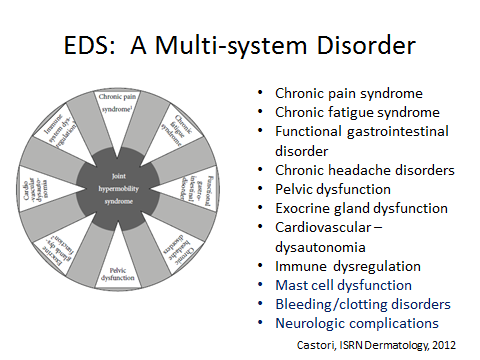
Ehlers-Danlos Syndrome Joint Hypermobility (“EDS/JHM”)And Comorbidities including
Postural Orthostatic Tachycardia Syndrome and Dysautonomia
![]()
Where Quality of Life Meets The Art and Science of Medicine
EDUCATION ![]() CALL TO ACTION
CALL TO ACTION ![]() STRATEGY
STRATEGY
ILC DDD/EDS Program Co-Chairs
Dr. Norm Buckley, Dr. Juan Guzman, Dr. Fraser Henderson, Dr. Gail Ouellette,
Executive Summary – ILC Scientific Workshop Outcomes
The ILC Foundation, through its medical advisors, has identified the need to organize a more imminent and pragmatic approach to diagnoses, treatment and care of patients suffering from chronic pain, beginning with Ehlers-Danlos Syndrome (EDS), utilizing the updated clinical presentation of EDS, rather than the genetic molecular testing, currently in use.
The scientific workshop concluded that a pragmatic approach will enable family practitioners and front line medical care providers to better meet the need of this patient population. (While the molecular presentation of connective tissue disorders are critically important to the further understanding of this disease, which can also lead to potential cures in the fullness of time, it was determined that it was untenable to let these children, adolescents and young adults, and their families, suffer in pain and suffer the economic consequences as a whole).
On October 4th and 5th 2013, the ILC hosted the EDS scientific workshop. More than two dozen doctors and allied health professionals attended from Halton, Hamilton, London, the GTA, Quebec and the United States, to share knowledge, current best practices and information on EDS symptoms and treatments.
The ILC’s Difficult to Diagnose Disease Program (ILC-DDD Program) as a template-able model, was reviewed as a way to advance diagnostics, treatment and care of a broad group of chronic pain diseases where best practices do not exist, beginning with EDS; and, as a way to address the very challenging transition of care from child to adult once patients turn 18 years old.
The following presentations listed below took place at the scientific workshop. A question and answer period followed each presentation, which generated broader awareness and education.
- Revisiting a 100-Year Old Disease – Ehlers-Danlos Syndrome, Dr. Gail Ouellette, Ph.D. CGAC, Director, Quebec Coalition of Orphan Diseases
- Connective Tissues: A Genetic Review, Dr. Roberto Mendoza
- Clinical Presentation of Ehlers-Danlos Syndrome, Dr. Clair Francomano
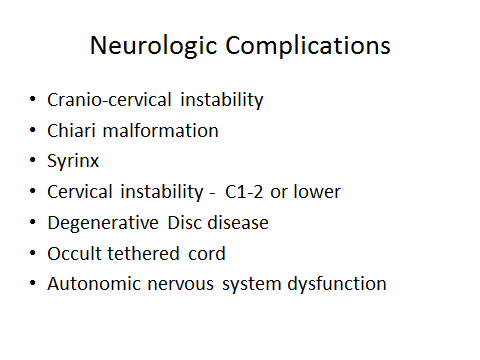
- Cervical Instability, Tethered Cord, Haematology and the difference in neuroradiology measurements in connective tissue disorders, Dr. Fraser Henderson
- Postural Orthostatic Tachycardia Syndrome and Dysautonomia, Dr. J. Guzman
- A Unique Pain Management Treatment for EDS Patients: A Manual Therapy Approach, Dr. Michael Healy
- Patient and Parent Presentations Re: The Impact of Misdiagnoses: Living with Chronic Pain & No Answers
- Heather (Mother)
- Brittany
- Emma
- Erika
- Erin
- Justin (read by Heather in Justin’s absence)
- Rebecca
BEST PRACTICES FOR DIAGNOSES – Physician notes and recommendations
- The value of identifying symptoms may lead to a diagnosis; it may be that it can help prevent harm from occurring because of inappropriate and slow to-come treatment interventions.
- The current referral process includes long wait lists and in succession specialist appointments; suggestion, which is a good one: that family physicians submit all referrals at once based on the new diagnoses criteria.
- Diagnoses should also lead to specific inquiry towards other manifestations eg: mast cell which can be addressed.
- Family physicians should coordinate care via multidisciplinary team at a major center when the following five to eight symptoms of the connective tissue are present, which may lead to a diagnosis of EDS/JHM.
- Dr. Francomano has data collected of over 300 EDS patients on the natural history to enable an updated clinical diagnosis; to understand what works and doesn’t work as treatment options.
- Rehabilitation medicine: Dr. Faroog Ismail (Westpark Clinic)
- Cardiology: Dr. Jack Colman (Connective Tissue specialist, TGH)
- Pain: Both Wasser Pain Center and Pain Clinic at St. Mike’s have shorter wait lists
- Ophthalmology: To rule out other connective tissue conditions
- Study to determine percentage of patients that have accidents to answer ‘what tips off’ condition. Could help to determine prevention strategies to maintain quality of life.
- Importance of self-management programs in Quebec; in Ontario programs vary from LIHN to LIHN; need to seek funding; integrate comprehensive peer support network.
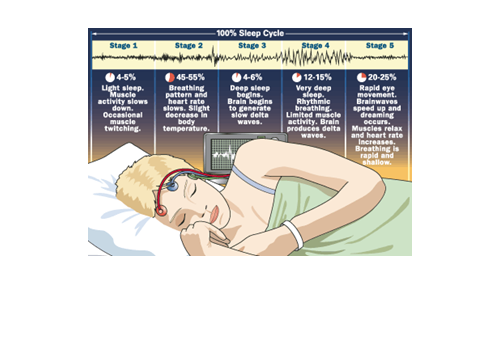
- Sleep study with beta blockers – seem to help
- Use of Aspen collar to determine if it helps with clinical symptoms of numbness, pain, dizziness. If it makes it worse, likely tethered cord
- What is the cost to society and cost to families
- Development of patient registry
- Questions to ask patients: What are the top three things mostly affected in quality of life and then help to determine how to help
- Centers of excellence for EDS care useful to triage / coordinate care plan
- Young patients attending virtual school / lack of social functioning / increased isolation
- Diagnosis helps to reduce harm from wrong treatment plan.
- Value to non-pharma and participate in psychological support to deal with pain and living with chronic illness
- Controlled clinical trial discussed in Ghent on cognitive based therapy
- ILC qualified resource impart on families /societal challenges/ Important to move patients through system faster when poly system complaints to lead person and continue to collect data.
- Question of molecular genetics leading diagnostics and treatment plans responded with ‘we have expertise present and there are experts with significant data including registry in France.
- Association of Family Practitioners Scientific Conference – Future planning around CME would be good to invite genetic talk
- Family practitioners would benefit greatly from knowing list of appropriate questions to ask patients.
- Collegial working relationships utilizing the KISS method of messaging
- Would be helpful for each participant to write a position paper of ‘what, when, where, why and how’ for EDS care
- Would be helpful to have data-base list of names to refer to.
- Generate list of contacts to give patients including ‘preferred provider’ for optimal treatment
EDS: WHAT IT IS?
KEY SYMPTOMS
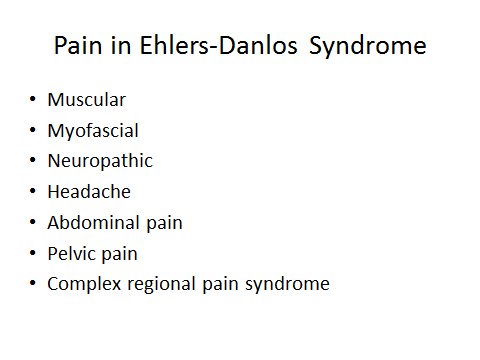
- Chronic widespread pain including chronic headache
- Bladder dysfunction
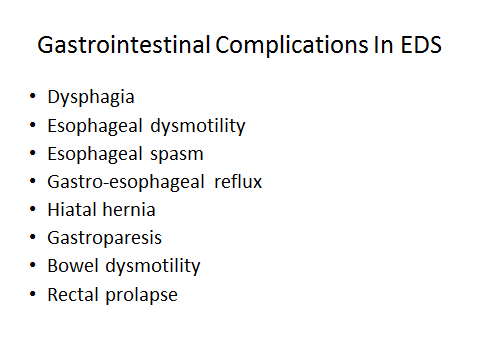
- GI complaints
- Syncope/pre-syncope
- Chronic fatigue
- Functional disability that is progressive and recurrent
- Joint and skin laxity
- Chronological variability and a family history
KEY REFERRALS
- PSYCHIATRY:
- To provide support because they do not have the tools to deal with that much pain when they are young.
- GENETICS:
- Whole family clinical and molecular genetic counselling to determine diagnosis.

- Brighton / Beighton Score
- Whole family clinical and molecular genetic counselling to determine diagnosis.
- NEUROLOGY:
- Rule out Chiari malformation
- Rule out cranial instability
- Rule out tethered cord and occult tethered cord (fatty filum of any kind, more often not recognized on MRI but rather a clinical presentation with the following clues: urodynamic that shows retention of any kind or residual retention or minor abnormalities especially evident in EDS patients)
- Rule out brain stem compression
- Identified in upright C-Spine weight bearing MRI (angel measurements)
- Rule out any kind of degenerative problems such as
- Identified in flexion extension MRI
- Rule out reflex odontoid basilar invagination at C1 (poking up in forum magnum into the panus or cerebellum causing brain
- Rule out any subluxation of c-spine, clivo axioal angel abnormalities (anything above 125 degrees)
- Identified in rotational ct scan – ear touching pillow/board one way and then the other for about 5 minutes each way (patient with EDS with confirmed presentation will be exhausted and feel very sick after this test).
- Identified in rotational ct scan – ear touching pillow/board one way and then the other for about 5 minutes each way (patient with EDS with confirmed presentation will be exhausted and feel very sick after this test).
- GASTROENTEROLOGY:
- CARDIOLOGY: (See presentation – Dr. Juan Guzman)
- To rule out Postural Orthostatic Tachycardia Syndrome (POTS)
- To rule out Postural Orthostatic Tachycardia Syndrome (POTS)
- HAEMATOLOGY:
- Determine vitamin D and iron deficiency
- Determine MTHFR gene presence
- Determine lupus antibodies
- Determine protein deficiencies and/or mutations
- ENDOCRINOLOGY:
- Determine if immune system is depressed
- Determine low cortisol levels which may explain sadness and low energy
- Determine if mast cell present
- ORTHOPEDICS/SPINE/NEUROSURGEON: (See presentation – Dr. Fraser Henderson)
- If cervical cranial instability or tethered cord – decompression can make it worse.
- Babies with EDS can present with
- acquired Chiari malformation because pulls on serabellum.
- Club foot
- dislocated hips
- 99.9% would not recognize cranial instability (Dr. Racati at the Chiari institute to confirm cranial instability.)
- If child had herniation beyond 7 or 8 ml should be seen by dr. racati – they recognize the relationship between EDS, Chiari and tethered cord. If they do find Chiari to do surgery, two years later herniation is worse as is Syringomyelia because in the process they are not recognizing tethered cord.
- Babies holding head, crying with headaches, bruising, brittle bones (vit D deficiency in Mom and baby)
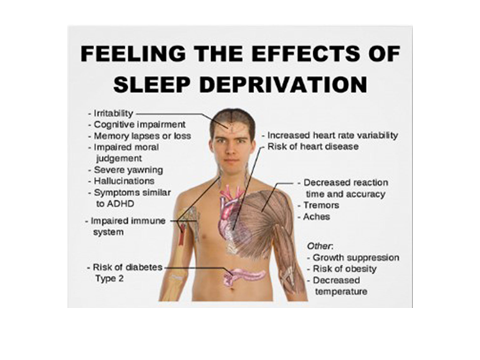
- SLEEP EXPERT:
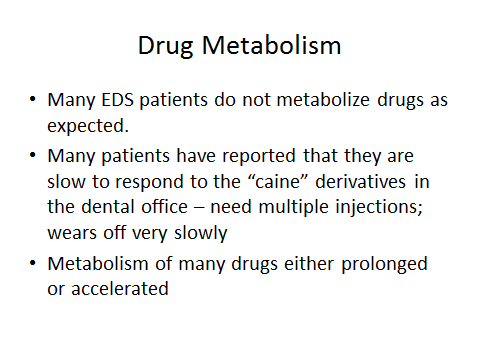
- PAIN SPECIALIST AND PHYSIOTHERAPY:
- PEER SUPPORT & RESOURCES NETWORK: (Visit – www.theilcfoundation.org)
- The ILC Foundation for peer support to replace feelings of isolation and fear with friendships and hope.
- The ILC Foundation for peer support to replace feelings of isolation and fear with friendships and hope.
Scientific Workshop Attendees
Dr. Norman (Norm) Buckley, MD, FRCPC, Anesthesiology, Co-Chair ILC DDD-EDS Program
Dr. Buckley Chair, Department of Anesthesia is an associate professor in the Department of Anesthesia of the Michael G. DeGroote School of Medicine, Faculty of Health Sciences at McMaster University and is the founder and director of the Pain Management Centre for Hamilton Health Sciences and McMaster University. Chair ILC Medical Advisory Board.
Dr. Juan Camilo Guzman, M.D. MSc, FRCPC, Cardiology, Co-Chair ILC DDD-EDS Program
Dr. Guzman is an Assistant Professor of Medicine at McMaster University and Internal Medicine specialist at Hamilton Health Sciences (Hamilton General Hospital Clinical Teaching Unit). After graduating from medical school in Colombia, Dr. Guzman completed a three year Clinical Research Fellowship in Autonomic Disorders at McMaster University in 2007, this was followed by 3 year residency training in Internal Medicine at McMaster University and 1 year of General Internal Medicine Fellowship. He holds a Masters of Sciences degree in Health Research Methodology from McMaster University. He received the Have a Heart Bursary Program Award by the Canadian Cardiovascular Society Academy in 2009 as young promising clinical researcher in Cardiovascular Sciences. He is a fellow of the Royal College of Physicians and Surgeons of Canada and he is a board certified Internal Medicine specialist. He has clinical and research interest in Syncope and Autonomic Disorders such as Pure Autonomic Failure, Multiple Syncope Atrophy, Postural Orthostatic Tachycardia Syndrome and Vasovagal Syncope. He is staff member of the Syncope and Autonomic Disorders Unit as well as the Autonomic Laboratory affiliated to the Arrhythmia Service at the Hamilton General Hospital. Dr. Guzman has published peer review articles, abstracts, and book chapters and has presented his work in multiple meetings around the world. Dr. Guzman has strong interest in medical education at the graduate and postgraduate level as well as knowledge translation from the teaching hospital to the general practitioner. Dr. Guzman is an active member of the Canadian Cardiovascular Society, American Autonomic Society and the Canadian Society of Internal Medicine. Co-Chair ILC DDD-EDS Program.
Dr. Fraser Cummins Henderson Sr. MD, Neurosurgeon, Co-Chair ILC DDD-EDS Program
Dr. Henderson was foreman on a cattle station in the Outback of Australia before receiving his bachelor’s and Medical degree at the University of Virginia, Charlottesville VA. He served for with the Multi-National Peace Keeping Force in Beirut, earning the Navy Commendation Medal for preparedness of and treatment of mass casualties following the terrorist bombing attack in Beirut, Lebanon , October1983. After completing his residency under Phanor Perot at the Medical University of South Carolina, he returned to complete his active duty obligation at the National Naval Medical Center, Bethesda, MD, as Director of Spine. He was Brigade Neurosurgeon for the 4th Marine Expeditionary Brigade in Desert Shield and Desert Storm during the 1st Gulf War. He then completed a fellowship in Craniospinal surgery under Professor Alan Crockard at The National Hospital for Neurology and Neurosurgery, Queen Square, London. Finishing his tour with the US Navy, Commander Henderson joined Georgetown University, in Washington D.C. as Director of Neurosurgery of the Spine and Cranio-cervical Junction. He was Co-Director of the Lombardi Neuro-Oncology Division, Co-Director of the CyberKnife Radiosurgery Center, and Medical Director of the Neuroscience Nursing Units. He was Professor of Neurosurgery and Radiology at Georgetown University, where he was active in advancing CyberKnife radiosurgery for treatment of chordoma and other complex spinal tumors. He developed intellectual property for three inventions relating to spinal radiosurgery and spinal cancer, including the TPS® –Telescopic Plate Spacer- a vertebral replacement device for metastatic disease and was Principal Investigator in the translational development of a radio-sensitizing drug, and a drug to block the malignant invasiveness of Glioblastoma Multiforme.
Dr. Henderson entered private practice in Bethesda Maryland, as Director of Neurosurgery at Doctors Hospital and Director of the Chiari Center of Excellence, where he is focused on the development of the understanding and treatment of deformity induced injury to the brainstem and spinal cord in Chiari Malformation and Ehlers Danlos Syndrome. He is inventor of 11 devices and concepts relating to disorders of the brainstem and spinal cord, has published over 50 peer reviewed articles and book chapters, and given over 130 invited lectures with a focus on craniocervical disorders, Chiari malformation, cancer, radiosurgery and unusual problems of the spine. Dr Henderson lives with his wife, Becky, and three sons- Fraser, Lansdale and Landon- on a farm in Prince Georges County, Maryland.
Dr. Clair Francomano, MD, Medical Genetics
Dr. Francomano received her undergraduate degree at Yale University and her medical degree from The Johns Hopkins University School of Medicine. She trained in internal medicine and medical genetics at Johns Hopkins and joined the full-time Hopkins faculty in 1984. She joined GBMC’s Harvey Institute of Human Genetics in 2005. Dr. Francomano is an Associate Professor of Medicine at Johns Hopkins University School of Medicine. She has held positions as Clinical Director and Chief of the Medical Genetics Branch at the National Human Genome Research Institute, National Institutes of Health and Chief of the Human Genetics and Integrative Medicine Section in the Laboratory of Genetics, National Institute on Aging. Dr. Francomano is board-certified in internal medicine, clinical genetics and clinical molecular genetics. She is a member of the American College of Physicians, the American Society of Human Genetics and the American Society for Clinical Investigation, and is a founding fellow of the American College of Medical Genetics. In 2008, and every year since, Dr. Francomano has been named among “Baltimore’s Best Medical Geneticists” by Baltimore Magazine. Her clinical and research interests include the hereditary disorders of connective tissue and skeletal dysplasias. She received EDNF’s Shining Star award in 2012 for her dedication to people with EDS.
Dr. Kristianna Martiniuk, MD
Dr. Martiniuk is Lead Physician at the Trafalgar Sheddon Family Health Organization and is an active staff member at Oakville Trafalgar Memorial Hospital with privileges in Obstetrics, Surgical assists, Pediatrics, Maternal-child committee member. In addition to her dedication to her patients, Dr. Martiniuk offers her expertise as the site lead for EMR implementation to support the entire practice. As Fellow, the Ontario College of Family Physicians, Dr. Martiniuk’s dedication includes Family Physician Mentor Collaborative Stroke Care. Dr. Martiniuk lives within the Halton Region and is married with 4 children.
Christina Pridmore, R.Kin
Registered Kinesiologist, Certified Pilates Instructor, Osteopathy (graduate student)
Christina is a Registered Kinesiologist, a Certified Stott Pilates Instructor, and graduated as Valedictorian of her class at the Canadian College of Osteopathy in Toronto. She has over twenty years’ experience in rehabilitative exercise therapy, with a specialty in the area of mind-body awareness.
Christina’s treatment philosophy involves a continuum of care, incorporating both manual therapy and therapeutic exercise, to help patients reach their individual goals.
Christina works with people of all ages and abilities with a particular interest in Pediatric Osteopathy. She is currently working on her post-graduate thesis entitled, “The effect of osteopathic treatment on visual accommodation in children aged 9-16 years”.
Dr. Peter B. Dent, MD, DCH, FRCPC
Dr. Dent, who is currently Professor Emeritus in the Department of Pediatrics at McMaster University, graduated from the University of Toronto Medical School in 1960. He trained in pediatrics at the Hospital for Sick Children in Toronto and Birmingham (UK) Children’s Hospital. He then did a research fellowship in immunology and rheumatology at the University of Minnesota specializing in cancer immunology. Supported by a Research Career Award from the Leukemia Society of America, he joined the Department of Pediatrics at McMaster University in 1968 where he established the Division of Rheumatology and Immunology. He became Chair of the Department in 1980 and served until 1990 during which time he founded the McMaster Children’s Hospital and he spearheaded the development of the local Ronald McDonald House, achievements for which he was inducted into the Hamilton Gallery of Distinction in 2008.
Subsequently, he served as Vice President (Medicine) for Chedoke McMaster Hospitals, as well as Director of Research for Hamilton Health Sciences from 1990 to 1997. In 2002, he became Associate Vice President (Clinical Services) for the Faculty of Health Sciences.
In the past, he served on the Executive of the Canadian Pediatric Society and he was President of the Assembly of Canadian Pediatric Department Chairman. He has also served as Chair of the Section of Pediatric Rheumatology of the American College of Rheumatology and on the sub-board of Rheumatology of the American Board of Pediatrics. In 2004, he received the James T. Cassidy Award for excellence in teaching and patient care in pediatric rheumatology from the American Academy of Pediatrics and in the same year became a Master of the American College of Rheumatology. In 2012 he will receive the Alan Ross Award which is given by the Canadian Pediatric Society to recognize lifelong excellence in the fields of pediatric research, education, health care and advocacy.
Dr. Dent’s continuing activities include the care of children with rheumatologic and immune deficiency diseases, medical administration and education, and clinical research in pediatric rheumatology.
Dr. Julie Richer, MD
Dr. Richer is a clinical medical geneticist at the Children’s Hospital of Eastern Ontario and an assistant professor at the University of Ottawa. Her clinical practice consists of general genetics with a particular interest in patients with heritable connective tissue disorders such as EDS and genetic conditions associated with thoracic aneurysms. Dr. Richer completed medical school at L’Université de Montreal, FRCPC in Medical Genetics at the University of Manitoba and a Fellowship in Medical Ethics at Harvard University. Dr. Richer is particularly interested in ethical issues related to genetic testing and utilization of genetic material in research. Her main areas of interest include perception of risk and issues related to disclosure of results derived from research using untargeted genetic testing.
Dr. Dora Mesec P.T. BSc
Dr. Mesec is a Certified Orthopaedic Manual Therapist, Certified IMS Gunn Practitioner, working in private practice, concentrating on musculoskeletal conditions with thirty year’s experience.
Dr. Michael P. Healy, PT, DPT, DOMTP, CSN, CPT, TPI, MBA
Dr. Healy, has been a practicing physical therapist for the past 27 years. He is currently in private practice and is the President and CEO of Healy Physical Therapy & Sports Medicine, Inc. in Rhode Island, NY. Dr. Healy’s specialty is advanced manual therapy with a personal interest in Ehlers Danlos Syndrome (EDS) patients. He combines biomechanics with the natural healing power of your body to assist in correcting any mal-alignments. “Once I stabilize and EDS patient’s body I enjoy teaching them correct core stabilization exercises.”
Education: 1.) University of New England; Bachelors’ Degree in Physical Therapy, 1986; 2.) Bryant University (formally known as Bryant College); MBA, 1997; 3.) American Muscle & Fitness Personal Training Institute; Sports Nutritionist Certified (CSN), 2003; 4.) American Muscle & Fitness Personal Training Institute; Personal Trainer Certified (CPT), 2003; 5.) Titleist Performance Institute (TPI); TPI Certified Golf Fitness Instructor, 2007.
6.) Osteopathic College of Ontario; Diplomate in Osteopathic Manipulative Theory & Practice, DOMTP, 2008.
7.) Simmons College; Doctor of Physical Therapy, DPT, 2013.
Jennifer Tyrrell RN, MN, Department of Anesthesia and Pain Medicine
Ms. Tyrrell is a Clinical Nurse Specialist in the Chronic Pain Clinic at The Hospital for Sick Children. Jennifer works with members of a multidisciplinary team to assess and provide support to children with chronic pain and their families. Jennifer is a member of the Canadian Pain Society and the International Association for the Study of Pain.
Dr. Roberto Mendoza-Londono, M.D., M.Sc, FCCMG, FRCPSC
Dr. Mendoza-Londono is a clinical geneticist in the Division of Clinical and Metabolic Genetics, Hospital for Sick Children and and associate professor the Departments of Paediatrics and Molecular Genetics, University of Toronto. He is a member of the steering committee for The Bone Health Centre and a project investigator at the Research Institute, Hospital for Sick Children. His clinical/research interests are in the areas of skeletal dysplasias, connective tissue and metabolic bone disorders.
Dr. Howard H.W. Chan, M.B.Ch.B., M.Sc., FRCP(C),
Dr. Chan is an Assistant Professor at McMaster University in the Department of Medicine in the Division of Hematology. He received M.B.Ch.B. at The Chinese University of Hong Kong in 1987. He had 6-year oncology training at the Prince of Wales Hospital in Hong Kong. He immigrated to Canada in 1993 and recertified through International Medical Graduate (IMG) program. Dr. Chan then did internal medicine and hematology training at McMaster University in Hamilton. After that, Dr. Chan was a fellow in Transfusion Medicine Research Program, funded by Canadian Blood Service. He obtained M.Sc. in Medical Sciences in 2006.
Dr. Chan’s overall research interest is the pathophysiology of thromboembolism, focusing on the interactions of fibrinogen with divalent cations and other proteins. His current research activities are in the following areas:
- effects of zinc on fibrinogen and heparinheparin co-factor in the treatment of thromboembolism
- autoimmunity of glucose-regulated protein 78
These researches involve studies at the levels of molecular biology, protein biochemistry, cell biology and experimental animal models. Dr. Chan’s recent publications include reviews in “Mechanisms in Hematology” and a peer-review paper of the works on fibrin-bound thrombin. The results of the study were selected for an oral presentation in a special symposium in American Society of Hematology 2007.
Dr. Hanna Faghfoury, MDCM, FRCPC, FCCMG
Dr. Faghfoury is Assistant Professor of Medicine, University of Toronto, Staff, Clinical and Metabolic Genetics, The Fred A. Litwin and Family Centre in Genetic Medicine, University Health Network and Mount Sinai Hospital
Dr. Chumei Li, MD, PhD, Genetics
Dr. Li is an Associate Professor in the Department of Pediatrics at McMaster University. She obtained her medical degree in China and her PhD from the University of Toronto, winning the most distinguished dissertation award for life sciences at U of T for 1995-1997. She also trained in clinical cytogenetics and clinical genetics at the University of Toronto and University of Manitoba. She is a fellow of the Royal College of Physicians and Surgeons of Canada and the Canadian College of Medical Geneticists.
Dr. Li’s interests include genetic syndromes of overgrowth and failure-to-thrive/short stature, clinical dysmorphology and knowledge translation research.
Dr. Gail Ouellette, Ph.D. CGAC
Dr. Ouellette is the founder and the president of the Quebec Coalition of Orphan Diseases (Regroupement québécois des maladies orphelines) and of the Info Portal on Orphan Diseases. She obtained her Ph.D. in molecular genetics at the Université de Montréal. She did her postdoctoral studies in genetic epidemiology at the Centre for Human Genetics in Leuven, Belgium. She was a researcher at Algene Biotechnologies and Signalgene where she worked in gene discovery for compex diseases in founder populations. In 1999, she left the laboratory and the computer to train for a Master’s in Genetic Counselling at McGill University in order to do clinical genetics. She worked as a genetic counsellor at the Centre hospitalier universitaire of Sherbrooke and at Procréa Cliniques in Montreal. Since 2005, she has been involved as a volunteer consultant with various patient organizations in Quebec and Canada. Since 2010, she devotes all of her time to the Quebec Coalition of Orphan Diseases. Regroupement québécois des maladies orphelines, Portail Info Maladies Rares Québec.
Dr. Peter Vadas, MD PhD FRCPC (Regrets – On-Distribution)
Dr. Vadas is the Director Division of Allergy and Clinical Immunology at St. Michael’s Hospital. Dr. Vadas sends his apologies for having to decline. “The program and scheduled speakers for the Scientific Workshop are outstanding and I would dearly love to take part because the topics are ones that rarely make their way onto scientific programs.”
Dr. Adam Chen – Acupuncturist and TCM
Dr. Chen is one of Canada’s leading acupuncture specialists, Dr. Chen is the founder of the acupuncture clinic at Mount Sinai Hospital. Dr. Chen’s clinical work focuses on pain management and women’s health issues and has been frequently called upon by government agencies to provide expertise on Traditional Chinese Medicine. His pioneer work of introducing acupuncture into Canadian hospitals have been featured in variety of media outlets. – See more at: https://www.mountsinai.on.ca/wellbeing/biographies/biographies/dr-adam-chen#sthash.pvk8zExd.dpuf.
Dr. Mohammed F. Shamji – MD, PhD, FRCSC, FAANS (Regrets. On Distribution)
Dr. Shamji is a Staff Neurosurgeon at Toronto Western Hospital and Assistant Professor at the University of Toronto. (Regrets, on distribution for following collaboration)
Dr. James H Eubanks, PhD
Dr. Eubanks is Senior Scientist and Scientific Division Head of Research, Division of Genetics & Development at the Toronto Western Research Institute (TWRI). Dr. Eubanks interest is in stoke, epilepsy, Rett Syndrome, neurodegeneration and epigenetics. Dr. Eubanks is also a medical advisory board member with the Ehlers-Danlos Syndrome Ontario support network.
Dr. Allan Gordon, MD
Dr. Gordon is the Neurologist and Co-Medical Director of the Wasser Pain Management Centre at Mount Sinai Hospital (MSH). He graduated from the University of Toronto in Medicine and trained in Toronto, attaining his fellowship in Neurology. He has been a neurology consultant at MSH since 1974 and Head of Neurology at Mount Sinai since 1980. He is an Associate Professor at the University of Toronto and has served as Director of Development and later Assistant Dean of Development in the Faculty of Medicine. Dr. Gordon established the Craniofacial Pain Research Unit devoted to the diagnosis and treatment of people with facial pain and headache. This unit has since grown to become the Wasser Pain Management Centre.
Dr. Peter H. Byers, MD
Dr. Byers is a graduate of Reed College and Case Western Reserve University School of Medicine. Peter H. Byers trained in internal medical at the University of California, San Francisco and was a research associate at the National Institutes of Health in Bethesda, MD. He went to the University of Washington, Seattle, in 1974 as a fellow in medical genetics and biochemistry. He joined the faculty in 1977 and became a full professor in the Departments of Pathology and Medicine (Medical Genetics) in 1986. Byers is past president of the American Society of Human Genetics and of the American Board of Medical Genetics, and he served as editor of the American Journal of Human Genetics from 1993 to 1999.Byers is a founding member of the National Marfan Foundation Professional Advisory Board, a member of the Medical Advisory Council of the Osteogenesis Imperfecta Foundation, which he chaired for five years, and has been a member of the Ehlers-Danlos National Foundation medical advisory group. He is the Director of the Collagen Diagnostic Laboratory at the University of Washington. He received the March of Dimes/Colonel Harland Sanders Award for lifetime achievement in the field of genetic sciences.
Dr. Clive Davis – MD, FRCPC
Dr. Davis is Associate Clinical Professor Internal Medicine, Hamilton General Hospital, Divisions of Critical Care, Respirology, and General Internal Medicine, Department of Medicine, Hamilton General Hospital.
Howard Meng is a 4th year medical student from the University of Toronto with a strong interest in anesthesia and chronic pain management. He has authored student publications in these areas. He is currently engaged in research activities at the Wasser Pain Management Centre at Mount Sinai Hospital in Toronto.
Dr. Serge B. Melancon, MD, FRCPC, FCCMG, Medical Genetics and Pediatrician
Dr. Meloncon is the Medical and Biochemical Generics Director, Department of Medical Genetics and Biochemical Genetic Services at the University of Montreal. He is also the Coordinator medical d-Orphanet au Quebec. Fellowship(s): Biochemical Genetics, Department of Pharmacology, University of British Columbia; Northwestern University Medical School Clinical Training Division, Chicago, Illinois, The Children’s Memorial Hospital, Chicago, Illinois. Research interests: Hereditary Ataxias, Neurodegenerative and Lysosome Storage Disorders.
Daisy Rusi Pavri, MD, Pediatrician
UNIVERSITY AFFILIATIONS
- Adjunct Professor at Western University, London, Ontario
- Victoria Hospital (CHWO) – Part time staff with admitting privileges
- St. Joseph Hospital – Part time consulting staff with admitting privileges 1984 – 2011
- CPRI – Consulting staff, mainly with the Home Visiting Program for Infants (HVPI) 1984 – 1996
- LMCC Examiner for more than 15 years.
- Volunteering in the interviewing process for Admissions – Schulich School of Medicine and Dentistry 1999 onwards
- CEHPEA – Centre for the Evaluation of Health Professionals Educated Abroad – as an examiner for OSCE Stations and writing exam questions – 2008 and 2009.
POSTGRADUATE TRAINING
- March 1978 – December 1978. Rotating Internship for TNMC, in Preventive and Social Medicine, Surgery, Obstetrics & Gynaecology, India.
- December 1978 – March 1979. Rotating Internship for TNMC, in Medicine (as a special case – Observer Status), London, Ontario
- May 1979 – June 1979 (6 weeks), Paediatric Intern, Victoria Hospital, University of Western Ontario, London, Ontario
- July 1979 – June 1980. Resident I, Paediatrics, Hospital for Sick Children, University of Toronto, Toronto, Ontario.
- July 1980 – June 1981. Resident II, Paediatrics, Hospital for Sick Children, University of Toronto, Toronto, Ontario.
- July 1981 – June 1982. Resident III, Paediatrics, Victoria Hospital, University of Western Ontario, Ontario.
- July 1982 – June 1983. Perinatal Fellow, Regional Perinatal Unit, Women’s College Hospital, University of Toronto, Toronto, Ontario.
- July 1983 – July 1984. Teaching Fellow, Paediatrics, Victoria Hospital, University of Western Ontario, London, Ontario.
MEDICAL CERTIFICATION
- 1979 M. B. M. B.S., Bombay, India
- 1979 E. C. F. M. G.
- 1982 M. C. C. E. E.
- 1983 L. M. C. C.
- 1983 Fellow, Royal College of Physicians and Surgeons of Canada
AWARDS AND PRIZES
- April 1977 (a) Shri Dongarshi SS. Karla’s Prize
- (b) Dr. W. B. Bhave Memorial Prise for securing highest marks among students of
- Topiwala National Medical College and Second M. B., B. S. Examination
- Sept. 1976 First prize in Essay Competition on Leprosy (in English) organized by Acworth
- Leprosy Hospital, Wadala, Bombay, for Inter-Medical Colleges of Bombay, India
- April 1977 Master Vishwanath Narayan Sambhu Scholarship on Competitive Examination in Surgery
- April 1977 Dr. N. V. Ajinkya Midwifery Medal in Competitive Examination in Obstetrics and Gynaecology
- July 1977 Dr. A. M. Gokhale Prize for standing first in Ophthalmology Inter-Municipal Medical Competition Examination
- Nov. 1977 Dr. A. L. Nair and M. Venkatro Cash Prize (equally shared with another student) for
- Securing highest mark in Surgery amongst the students of T. N. M. College at Third M. B., B. S. University Examination.
- Feb. 1978 J. R. D. Tata Trust Merit Scholarship for Medical Students from June 1983 – Feb. 1978
- Feb. 1980 First recipient of the Lionel Ginsler Memorial Scholarship. Variety Village, Variety Club
- of Ontario, for research related to the physically disabled child.
- Nov. 2004 Long Service Awards – London Health Sciences Centre – 20 years
- 2004 – 2005 University Students’ Council Teaching Honour Roll, UWO, London, ON.
- Oct. 2007 Award of Recognition for exemplary medical service to individuals with Cerebral Palsy.
PUBLICATIONS
- Pavri, D., Marshall D., Armstrong, R., Gorodzinsky F., : Intrauterine intussusceptions – A case report
- And review of the literature. Canadian Journal of Surgery, Vol. 26: # 4K, July 1983
- Pavri, D., “Malnutrition and Mental Development” – an article in CPRI Profile, Published quarterly by CPRI, Vol. 7: #1. 1986
- Consultant to HVPI Newsletter – “Infant Cryer” (a quarterly publication) – submitted articles of
- Interest for parents, E. C. E. Staff & CPRI staff.
ACADEMIC LECTURES/SEMINARS
- Presented lecture in Windsor, May 1987 re: Investigation and management of developmental delay (for general practitioners and 2 local paediatricians).
- Ottawa AAMD Conference in February 1988 – presented my paper on Atlanto – Axial Instability in Down Syndrome population.
- Presented lecture in Stratford, March 1991 as a continuing medical education experience for 2 paediatricians, family doctors, nurses and other health care professionals.
- Topics covered:
- Developmental delay (physical markers including slides)
- Down Syndrome – current research
- Interesting cases referred from Perth County
- Presented Lecture in Chatham, May 1991 – Developmental Paediatrics including Learning Disability (at Kent County Children’s Treatment Centre).
- Chairperson for Breast Feeding Committee – London and Middlesex Area – 1990’s
- Presented Lecture at Presidente Prudente University, Brazil for Medical Students on Aug. 16, 2001.
- Poster Presentation at Sao Paulo, Brazil Aug. 11 to 14, 2001 Unusual Fetal Chest Mass.
- Lecture Series for Abbott Laboratories: (Sponsored)
- – Iron nutrition in infancy (London and Sarnia 2003)
- – Infant feeding problems – the clinical challenges ( London) 2003-2004
- Developmental problems and skin rashes – Lecture for London Area Family Doctors in 2004
- Presented Teaching Seminar, February 1992 – Petrolia. Attention Deficit Disorder – 1 day seminar for teachers and parents.
- Presented Teaching Seminar, April 1992 – CPRI., London, Ontario. Infant Development – 1 day seminar for teachers, E. C. E. Workers and Infant Therapist.
- Ongoing teachings for IMG and overseas medical students in office and the local community.
- Ongoing teaching in India for residents in Paediatrics.
Dafna Bena
Dafna Bena graduated from physiotherapy in 1993 from Istanbul University, Turkey. In 1994, she moved to Israel and completed her Masters of Neuroscience in Neurobiology in 2003 from Hebrew University Jerusalem. Additionally, Dafna is trained in advanced chest physiotherapy, critical care treatments, hydrotherapy and Aquatic therapy courses, including infant courses, Bobath-NDT therapist, Leadership and Advanced Leadership courses and many more. Dafna has extensive experience in pediatric rehabilitation, critical care with various populations of head injuries, Cerebral Palsy, Spinabifida, Familial Dysautonomia, neuromuscular Disorders, numerous different and very rare syndromes, spinal cord injuries, respiratory issues and chest physiotherapy for ventilated and non-ventilated pediatric patients (no respiratory therapists exist in Israel) and other unique traumatic conditions including suicide attack survivors. In 2004, Dafna moved to Canada and has worked mainly with adults in retirement homes, nursing homes; private clinics included orthopedic and mild neurological conditions such as concussions; and worked as in home assessor for car insurance–injuries. In the last 2 years, Dafna has been working as a pelvic health Therapists to help women and men suffering from various pelvic health conditions related to pain, incontinence and dysfunction. Dafna currently works at Hamilton Health Sciences in GIMRAC clinic and the Pediatric Cystic Fibrosis Clinic.
Ni Shen, Ph.D.
Ni Shen graduated from Xiangya school of medicine, Central South University in China and completed four years of Plastic Surgery residency training in China. Ni Shen obtained a Ph.D. degree on HIV research at McGill University in Montreal. Ni graduated from the first class of the Physician Assistant program at McMaster University and worked as a Physician Assistant at the General Internal Medicine floor for in- hospital patients at Hamilton General Hospital and currently is working as a Physician Assistant at the General Internal Medicine Rapid Assessment Clinic at MUMC.
C Ammendolia
Non-medical and allied health attendees:
ILC Foundation:
- Kris and Rebecca Mills, Inspiration and co-Founders
- Peter Reinhardt, Director
- Sandy Smeenk, Founder and Executive Director
- John Stevenson, Director
Canadian Pain Coalition:
- Lynn Cooper, President
- Sandra Gartz, Director

